What Is Revenue Cycle Management And What Are Its Benefits?
Organizations in every industry must ensure that enough revenue is generated to cover expenses. This is also true in the healthcare industry. Unfortunately, many healthcare organizations have difficulty collecting reimbursements on time, which can have a negative impact on the quality of care they provide to their patients.
Many hospitals and clinics operate with limited resources and time. Furthermore, many employees must perform multiple roles, making it nearly impossible to stay on top of all tasks without making mistakes.
Because many hospitals handle billing using inefficient manual processes, the most common billing issues are caused by human error, such as data entry errors.
This is why successful medical practices employ a revenue cycle management (RCM) programme, also known as a streamlined billing process. Healthcare organizations use rules-based software to ensure that they generate the revenue to which they are entitled as soon as possible.
Source- https://www.indeed.com/career-advice/career-development/what-is-revenue-cycle-management
What Is Revenue Cycle Management?
Revenue Cycle Management (RCM) is the process of identifying, collecting, and managing revenue from payers based on the services provided by the practice. A successful RCM process is critical for a healthcare practice to remain financially viable while also providing quality care to its patients.
The shift towards value-based reimbursement and more holistic patient care has compelled healthcare providers to reconsider their approach to revenue cycle management. Poor billing practices can lead to financial losses and jeopardize the ability to provide quality care. Efforts to improve and streamline core operational procedures can assist providers in remaining financially viable.
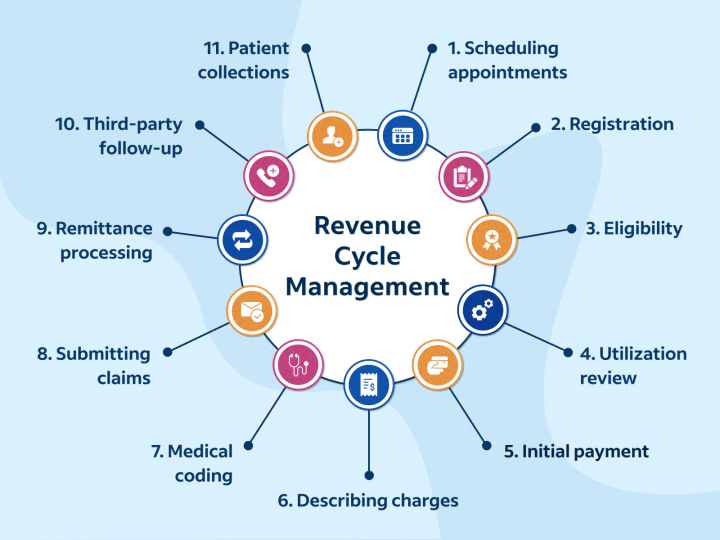
Revenue Cycle Management Process
RCM (revenue cycle management) is a critical process for healthcare providers that involves managing the financial aspects of a patient’s visit from appointment scheduling to payment collection. The revenue cycle management steps are critical to ensuring that healthcare providers are paid on time for the services they provide.
Making Appointments
Scheduling an appointment with the patient is the first step in the revenue cycle management process. This includes gathering personal and medical information from them, such as their name, date of birth, insurance information, and reason for the visit. The demand for virtual assistants is increasing, and one area where virtual receptionists excel at is appointment scheduling.
Registration of Patients
After making an appointment, the patient must fill out registration forms with demographic and medical information. This information is used to verify eligibility and benefits and to provide accurate billing.
Verification of Eligibility and Benefits
To determine their payment responsibility, healthcare providers must verify their patients’ insurance coverage and benefits. This includes reviewing the patient’s insurance policy for co-pays, deductibles, and other payment information.
Examination of utilization
Utilization review ensures that patients’ healthcare services are medically necessary and meet insurance coverage criteria. This review is carried out to avoid unnecessary treatments that could lead to claim denials or non-payment.
Authorization and Referral
Before receiving speciality care or services, some insurance plans require a referral or authorization from a primary care physician or insurance company. Before providing services, the healthcare provider must ensure that the patient has obtained the necessary referral or authorization.
Defining Charges
Healthcare providers are required to provide a detailed breakdown of the charges incurred during a patient’s visit. This includes any medical devices used, as well as any services provided.
Billing and Coding
The coding and billing process entails assigning appropriate codes to medical procedures and services in order to ensure that the claim accurately reflects the care provided. This procedure assists in avoiding claim denials or incorrect payments. With constant changes in billing codes and administrative practice personnel under constant pressure, ideal conditions for revenue leakage from the practice are created.
Charge Publication
Healthcare providers post charges to the patient’s account after billing the insurance company. This procedure ensures that the patient’s account balance is current.
Making a Claim
The healthcare provider submits the claim to the insurance company for payment once the charges have been posted.
Clearinghouse Rejections
Insurance companies sometimes deny claims because of incorrect coding or incomplete information. Clearinghouses are used by healthcare providers to track and manage claim denials.

Source- https://www.okeasylife.com/steps-of-revenue-cycle-management/
What is Healthcare Revenue Cycle Management?
Financial stability is critical for healthcare organizations to stay in the business of helping patients. To ensure profitability and long-term viability, they must effectively collect and manage revenue. Equally important is having full visibility into their revenue cycle and revenue generation practices, including billing, payment, and claims processing.
Healthcare revenue cycle management involves coordinating various administrative and clinical functions to optimize cash flow and reduce errors or delays in payment. With the increasing complexity of healthcare billing, leveraging Revenue Cycle Management Technology has become essential. These technologies automate key steps in the revenue cycle, improving accuracy, efficiency, and transparency.
By understanding and implementing effective revenue cycle management, healthcare providers can enjoy the numerous benefits of revenue cycle management, including improved financial health and the ability to focus more on delivering quality patient care.
Benefits Of Revenue Cycle Management In Healthcare
Let’s look at some of the most notable benefits of healthcare revenue cycle management:
Increase in Claims Paid Following Initial Submission
To ensure claims are paid the first time they are submitted, successful revenue cycle management places a premium on accurately completing front-end tasks. These front-end tasks include insurance verification, accurate patient information collection, and proper coding.
On average, between 5% and 10% of claims are denied after their initial submission. However, the majority of these denials are the result of human error and technical issues. These include coding and insurance verification errors, as well as missing information in the patient’s chart. In fact, approximately 90% of claim denials are avoidable.
When claims are denied, they can be bounced around for months between insurance companies and providers until all issues are resolved. The best way to avoid these costly delays is to ensure that the claims are correct before submitting them.
Increase your practice time Revenue and collection
Healthcare facilities must account for a wide range of expenses. They must not only pay for the services they provide to patients, but they must also pay their employees for the work they do. When claims are denied or patients are unable to pay for services in advance, payments to the healthcare facility are delayed. This makes it difficult for the practice to manage its expenses.
To avoid this, RCM assists practices in identifying patterns of claim denial. By recognizing these patterns, practices can work to avoid future claim denials and receive timely reimbursement.
Not only do denied claims cause reimbursement delays, but they also cost the provider money in claim investigations and appeals. In fact, practices spend an average of $15,000 reworking claims. As a result, effective claim denial prevention can generate more than $5 million in additional revenue for the average hospital.
Patient Experience Enhancement
With a greater emphasis on patient outcomes, effective revenue cycle management means better overall patient experience. Patients can expect more comprehensive and targeted care, which will reduce the likelihood of readmission.
RCM also streamlines processes such as scheduling, filling out intake forms, and billing, resulting in a more pleasant experience for both patients and administrative staff. Also, because RCM emphasizes thorough insurance verification from the start, patients will have a better understanding of their insurance eligibility from the start. That way, they won’t be surprised by any out-of-pocket expenses later on.
Reduced Administrative Burden
When a patient requests an appointment, the administrative staff is in charge of scheduling it, establishing or updating patient information, and, most importantly, verifying their insurance. These front-end tasks are streamlined with a revenue cycle management system, allowing administrative staff to work more efficiently.
Also, RCM ensures that these administrative tasks are completed correctly so that claims are not denied in the future. When claims are not denied, the administrative staff is relieved of the burden of investigating and appealing denials.
Also Read: Building a Continuum Workplace: Healthy Employee Engagement Practices
The Importance of Data in Revenue Cycle Management
Data is key to effective revenue cycle management. It bridges the business and clinical aspects of healthcare by uniting administrative data, including the patient’s name, insurance carrier, coverage, and personal data, with clinical data such as treatments, medical history, preconditions, allergies, and lab results. Together, this data provides an overall picture of the care and financial obligation of the patient.
Understanding what revenue cycle management means, recognizing the critical role data plays in every step of the process. A crucial part of managing the revenue cycle is creating a patient account that starts at the time of appointment scheduling. Preregistration, which means collecting patient information before they arrive, helps make the revenue cycle clearer and reduces the chance of mistakes or duplicated work. This process makes revenue cycle management more efficient.
Using accurate data along with Revenue Cycle Management Technology allows healthcare organizations to improve operations, reduce errors, and enjoy the benefits of revenue cycle management, such as faster payments and better financial results.
Challenges in Revenue Cycle Management
Healthcare organizations face several significant challenges in managing their revenue cycle effectively. Understanding these challenges is essential to unlocking the full benefits of revenue cycle management.
Managing Complex Patient Data and Claims Processing
One major challenge is handling large amounts of patient data alongside numerous insurance claims. When data is incorrect or overwhelming, errors occur that lead to delayed payments and lost revenue. Mistakes in claims processing or patient data management can be costly and time-consuming, making it difficult for healthcare providers to receive payments promptly and accurately.
Research shows that nearly 65 percent of claim denials come from errors in coding and patient data. This statistic highlights the importance of accurate data management in successful revenue cycle management. Using Revenue Cycle Management Technology to automate claims and data entry processes helps reduce errors, speeds up processing, and increases the chances of claims being accepted.
High Claim Denial Rates and Reimbursement Delays
Claim denials and delayed reimbursements create financial pressure and disrupt cash flow for healthcare providers. Common reasons for denials include coding mistakes, missing documentation, and insurance-related issues. Each denied claim means lost revenue and additional effort to correct and resubmit.
Industry data indicates that between 10 and 15 percent of claims are rejected or denied, emphasizing the need for effective denial management. Regular staff training and real-time monitoring of claims and coding help minimize errors, leading to faster claim approvals and improved revenue flow.
Staying Compliant with Changing Regulations
Healthcare regulations such as ICD-10, MACRA, and HIPAA frequently change. Failing to keep up with these changes can result in significant legal and financial penalties, sometimes costing healthcare providers millions of dollars.
Maintaining compliance requires continuous education and vigilance. Leveraging Revenue Cycle Management Technology that provides real-time updates on regulatory changes enables healthcare organizations to stay compliant and avoid costly fines.
Patient Payment Collection and Rising Out-of-Pocket Costs
With rising co-pays and deductibles, more patients are responsible for a larger portion of their healthcare costs. Over 70 percent of patients now face out-of-pocket expenses, which makes collecting payments more challenging for providers.
Healthcare organizations can improve collections by offering patient-friendly payment plans, convenient digital payment options, and clear communication about financial responsibilities. These steps help ensure steady revenue while supporting patients in managing their bills.
Inefficient Prior Authorization Processes
Prior authorization requires approval from insurance companies before certain services or treatments can be delivered. This process is often manual and slow, leading to delays in patient care and added administrative work.
Nearly 86 percent of healthcare providers report prior authorization as a burdensome process. Automating prior authorization with technology speeds up approvals, reduces paperwork, and improves patient care. This is an important step toward optimizing revenue cycle management.
Why Should Healthcare Facilities Use RCM Software Solutions?
Healthcare organizations nowadays are experiencing greater difficulty in effectively managing their revenue cycle. This is the reason most organizations are looking toward Revenue Cycle Management (RCM) software solutions in order to automate their processes and enhance financial performance.
Medical RCM software streamlines and automates many critical tasks, from scheduling appointments with accuracy to delivering accurate medical billing and coding. The accuracy ensures quicker processing of claims by insurers and enables healthcare providers to receive payments promptly. By processing patient information and billing electronically, RCM software executes these functions quicker, more accurately, and with less error than manual processes.
The application of sophisticated Revenue Cycle Management Technology minimizes the requirement for manual labor, allowing staff to concentrate on more-prioritized tasks that necessitate human input. This movement increases overall productivity and efficiency in operations.
Some key benefits of adopting RCM software solutions include:
- Reducing phone calls and hold times by automating eligibility verification and patient communications.
- Standardizing eligibility checks and prior authorizations through online payer systems, which reduces eligibility issues and increases the accuracy of billing “clean” claims.
- Keeping revenue teams informed about payer policies, billing requirements, and reimbursement criteria to minimize errors and delays.
- Providing up-to-date training on government regulations to help healthcare providers comply and avoid penalties.
- Improving patient payment collection with online portals that reduce phone calls, eliminate multiple statements, speed up payment posting, and shorten turnaround times.
Incorporating the latest RCM technology is essential for healthcare organizations seeking to maximize the benefits of revenue cycle management. These software solutions enhance accuracy, speed up claims processing, and help maintain steady cash flow, allowing providers to focus on delivering quality patient care.
Conclusion
Revenue Cycle Management (RCM) is a critical process that medical care providers depend on to efficiently handle their financial processes. It encompasses each step of the way, from patient registration to billing and payment collection. The advantages of revenue cycle management are better cash flow, reduced billing errors, increased patient satisfaction, and better financial decision-making. By streamlining revenue cycle management procedures, healthcare organizations can spend more time and resources on high-quality patient care. With integrating the latest Revenue Cycle Management Technology, new heights of accuracy and efficiency can be achieved. Join forces with ProHance and transform your workforce management and RCM now!
Frequently Asked Questions
Q1: What Healthcare Billing Trends Can We Expect?
Difficulties obtaining payer authorization will continue, so facilities must maintain clear medical records and documentation to facilitate prompt payment and avoid claim rejections. Other trends in healthcare billing to be expected in the near future include an increase in the use of automation and predictive analytics, as well as an increase in the use of cloud-based solutions.
Q2: What Are the Industry’s Most Serious Billing Challenges Right Now?
Obtaining authorizations from payers has proven to be the most difficult challenge for the industry. This is due to the rising cost of healthcare. As healthcare costs rise, many insurance companies are finding it difficult to keep up with claim payments, hence the emphasis on the need to justify extended inpatient stays or other costly treatment modalities. Other factors that could have hampered payer authorization include facilities billing for services that were not provided, overbilling services, or incorrect service coding.
Q3: How can ProHance help optimize our revenue cycle management?
ProHance helps you gain visibility into your team’s workflow and performance. It supports your existing Revenue Cycle Management Technology by reducing billing errors, improving claims accuracy, and increasing efficiency. With better control, you can experience the full benefits of revenue cycle management and improve financial outcomes.
Q4: What causes revenue loss in the healthcare revenue cycle?
You may face revenue loss due to inaccurate coding, incomplete patient data, missed deadlines, and denied claims. Without strong revenue cycle management, these issues can add up quickly. Using automated tools and proper staff training can help you avoid common mistakes and recover lost revenue.
Q5: What’s the difference between RCM and medical billing?
Medical billing is just one part of revenue cycle management. While billing focuses on claims and payments, revenue cycle management covers everything from scheduling and registration to collections and denial handling. By managing the full cycle, you can improve financial performance and reduce payment delays.
Q6: What role does workforce productivity play in revenue cycle management?
Your team’s productivity directly affects how well you manage the revenue cycle. When staff work efficiently, claims are processed faster and with fewer errors. Monitoring performance helps you spot issues early, stay on track with collections, and gain more benefits from revenue cycle management.






